Results 1 to 8 of 8
-
06-06-2010, 09:30 PM #1
Understanding Post Cycle Blood Tests
In need of PCBT's and stumped on how or what to exactly ask for? CMP's and LP's will give you what you need to know. Ask your doctor about these next time.
Comprehensive Metabolic Panel
Also known as: CMP; Chem 12; Chemistry panel; Chemistry screen; SMA 12; SMA 20; SMAC (somewhat outdated terms)
There is also a basic version of this Test but I would recommend this one.
What is it?
The Comprehensive Metabolic Panel (CMP) is a frequently ordered panel of tests that gives your doctor important information about the current status of your kidneys, liver, and electrolyte and acid/base balance as well as of your blood sugar and blood proteins. Abnormal results, and especially combinations of abnormal results, can indicate a problem that needs to be addressed. The CMP is typically a group of 14 specific tests that have been approved, named, and assigned a CPT code (a Current Procedural Terminology number) as a panel by Medicare, although labs may adjust the number of tests up or down. Since the majority of insurance companies also use these names and CPT codes in their claim processing, this grouping of tests has become standardized throughout the United States.
The CMP includes:
* Glucose
* Calcium
Both increased and decreased levels can be significant.
Proteins
* Albumin
* Total Protein
Albumin, a small protein produced in the liver, is the major protein in serum. Total protein measures albumin as well as all other proteins in serum. Both increases and decreases in these test results can be significant.
Electrolytes
* Sodium
* Potassium
* CO2 (carbon dioxide, bicarbonate)
* Chloride
The concentrations of sodium and potassium are tightly regulated by the body as is the balance between the four molecules. Electrolyte (and acid-base) imbalances can be present with a wide variety of acute and chronic illnesses. Chloride and CO2 tests are rarely ordered by themselves.
Kidney Tests
* BUN (blood urea nitrogen)
* Creatinine
BUN and creatinine are waste products filtered out of the blood by the kidneys. Increased concentrations in the blood may indicate a temporary or chronic decrease in kidney function. When not ordered as part of the CMP, they are still usually ordered together.
Liver Tests
* ALP (alkaline phosphatase)
* ALT (alanine amino transferase, also called SGPT)
* AST (aspartate amino transferase, also called SGOT)
* Bilirubin
ALP, ALT, and AST are enzymes found in the liver and other tissues. Bilirubin is a waste product produced by the liver as it breaks down and recycles aged red blood cells. All can be found in elevated concentrations in the blood with liver disease or dysfunction.
How is the sample collected for testing?
The CMP uses a tube of blood collected by inserting a needle into a vein in your arm. Ask your doctor whether you should be fasting for 10 to 12 hours prior to the blood draw. Depending on the reason for ordering the CMP, it may be drawn after fasting or on a random basis.
How is it used?
The CMP is used as a broad screening tool to evaluate organ function and check for conditions such as diabetes, liver disease, and kidney disease. The CMP may also be ordered to monitor known conditions, such as hypertension, and to monitor patients taking specific medications for any kidney- or liver-related side effects. If your doctor is interested in following two or more individual CMP components, he may order the entire CMP because it offers more information.
When is it ordered?
The CMP is routinely ordered as part of a blood work-up for a medical exam or yearly physical. Although it may be performed on a random basis, the CMP sample is usually collected after a 10 to 12 hour fast (no food or liquids other than water). While the individual tests are sensitive, they do not usually tell your doctor specifically what is wrong. Abnormal test results or groups of test results are usually followed up with other specific tests to confirm or rule out a suspected diagnosis.
Article Sources
NOTE: This article is based on research that utilizes the sources cited here as well as the collective experience of the Lab Tests Online Editorial Review Board. This article is periodically reviewed by the Editorial Board and may be updated as a result of the review. Any new sources cited will be added to the list and distinguished from the original sources used.
Sources Used in Current Review
Henry’s Clinical Diagnosis and Management by Laboratory Methods. 21st ed. McPherson R, Pincus M, eds. Philadelphia, PA: Saunders Elsevier: 2007, P. 147.
Quest Diagnostics. Chemistry Screen, Patient Health Library. Available online at Chemistry Screen - [Medical Test] - Quest Diagnostics Patient Health Library through Quest Diagnostics Incorporated: The world's leader in diagnostic testing, information, services, blood tests, and lab tests.. Accessed February 2009.
Sources Used in Previous Reviews
Thomas, Clayton L., Editor (1997). Taber’s Cyclopedic Medical Dictionary. F.A. Davis Company, Philadelphia, PA [18th Edition].
Pagana, Kathleen D. & Pagana, Timothy J. (2001). Mosby’s Diagnostic and Laboratory Test Reference 5th Edition: Mosby, Inc., Saint Louis, MO.
American Medical Association (2002). Current Procedural Terminology, cpt 2002, Standard Edition.
Lipid Profile
Also known as: Lipid Panel; Coronary Risk Panel
Formal name: Lipid Profile
Related tests: Cholesterol; HDL-C; LDL-C; Triglycerides; Direct LDL-C; VLDL-C; Cardiac Risk Assessment; Lp-PLA2
What is a lipid profile?
The lipid profile is a group of tests that are often ordered together to determine risk of coronary heart disease. They are tests that have been shown to be good indicators of whether someone is likely to have a heart attack or stroke caused by blockage of blood vessels or hardening of the arteries (atherosclerois). The lipid profile typically includes:
* Total cholesterol
* High density lipoprotein cholesterol (HDL-C) — often called good cholesterol
* Low density lipoprotein cholesterol (LDL-C) —often called bad cholesterol
* Triglycerides
An extended profile may also include:
* Very low density lipoprotein cholesterol (VLDL-C)
* Non-HDL-C
Sometimes the report will include additional calculated values such as the Cholesterol/HDL ratio or a risk score based on lipid profile results, age, sex, and other risk factors. Talk to your doctor about what these other reported values may mean for you.
How is the sample collected for testing?
A blood sample is obtained by inserting a needle into a vein in the arm. Sometimes a drop of blood is collected by puncturing the skin on a fingertip. This fingerstick sample is typically used when a lipid profile is being measured on a portable testing device, for example, at a health fair. You need to fast for 9-12 hours before having your blood drawn; only water is permitted.
How is a lipid profile used?
The lipid profile is used to help determine your risk of heart disease and to help guide you and your health care provider in deciding what treatment may be best for you if you have borderline or high risk. The results of the lipid profile are considered along with other known risk factors of heart disease to develop a plan of treatment and follow-up. Depending on your results and other risk factors, treatment options may involve life-style changes such as diet and exercise or lipid-lowering medications such as statins.
When is it ordered?
It is recommended that healthy adults with no other risk factors for heart disease be tested with a fasting lipid profile once every five years. You may be screened using only a cholesterol test and not a full lipid profile. However, if the cholesterol test result is high, you may have follow-up testing with a lipid profile.
If you have other risk factors or have had a high cholesterol level in the past, you should be tested more regularly and you should have a full lipid profile.
For children and adolescents at low risk, lipid testing is usually not ordered routinely. However, screening with a lipid profile is recommended for children and youths who are at an increased risk of developing heart disease as adults. Some of the risk factors are similar to those in adults and include a family history of heart disease or health problems such as diabetes, high blood pressure (hypertension), or being overweight. High-risk children should have their first lipid profile between 2 and 10 years old, according to the American Academy of Pediatrics. Children younger than 2 years old are too young to be tested.
A lipid profile may also be ordered at regular intervals to evaluate the success of lipid-lowering lifestyle changes such as diet and exercise or to determine the effectiveness of drug therapy such as statins.
What do the results mean?
In general, your doctor will take into consideration the results of each component of a lipid profile plus other risk factors to determine whether treatment is necessary and, if so, which treatment will best help you to lower your risk of heart disease. The National Cholesterol Education Program offers the following guidelines for adults for classifying results of the tests:
LDL Cholesterol
Optimal: Less than 100 mg/dL (2.59 mmol/L)
Near/above optimal: 100-129 mg/dL (2.59-3.34 mmol/L)
Borderline high: 130-159 mg/dL (3.37-4.12 mmol/L)
High: 160-189 mg/dL (4.15-4.90 mmol/L)
Very high: Greater than 190 mg/dL (4.90 mmol/L)
Total Cholesterol
Desirable: Less than 200 mg/dL (5.18 mmol/L)
Borderline high: 200-239 mg/dL (5.18 to 6.18 mmol/L)
High: 240 mg/dL (6.22 mmol/L) or higher
HDL Cholesterol
Low level, increased risk: Less than 40 mg/dL (1.0 mmol/L) for men and less than 50 mg/dL (1.3 mmol/L) for women
Average level, average risk: 40-50 mg/dL (1.0-1.3 mmol/L) for men and between 50-59 mg/dl (1.3-1.5 mmol/L) for women
High level, less than average risk: 60 mg/dL (1.55 mmol/L) or higher for both men and women
Fasting Triglycerides
Desirable: Less than 150 mg/dL (1.70 mmol/L)
Borderline high: 150-199 mg/dL(1.7-2.2 mmol/L)
High: 200-499 mg/dL (2.3-5.6 mmol/L)
Very high: Greater than 500 mg/dL (5.6 mmol/L)
The risk categories for children and adolescents are different than adults. Talk to your child’s pediatrician about your child’s results.
Common Questions
1. I had a screening test for cholesterol. It was less than 200 mg/dL (5.18 mmol/L). Do I need a lipid profile?
If your total cholesterol is below 200 (5.18 mmol/L) and you have no family history of heart disease or other risk factors, a full lipid profile is probably not necessary. However, an HDL-cholesterol measurement would be advisable to assure that you do not have a low HDL. Many screening programs now offer both cholesterol and HDL.
2. My lipid profile results came back with high triglycerides and no results for LDL-cholesterol. Why?
In most screening lipid profiles, LDL-cholesterol is calculated from the other lipid measurements. However, the calculation is not valid if triglycerides are over 400 mg/dL (4.52 mmol/L). To determine LDL-cholesterol when triglycerides are over 400 mg/dL (4.52 mmol/L) requires special testing techniques such as a direct LDL-C test or a lipid ultracentrifugation test (sometimes called a beta-quantification test).
3. What is VLDL?
Very Low Density Lipoprotein (VLDL) is one of three major lipoprotein particles. The other two are high density lipoprotein (HDL) and low density lipoprotein (LDL). Each one of these particles contains a mixture of cholesterol, protein, and triglyceride, but in varying amounts unique to each type of particle. LDL contains the highest amount of cholesterol. HDL contains the highest amount of protein. VLDL contains the highest amount of triglyceride. Since VLDL contains most of the circulating triglyceride and since the composition of the different particles is relatively constant, it is possible to estimate the amount of VLDL cholesterol by dividing the triglyceride value (in mg/dL) by 5. At present, there is no simple, direct way of measuring VLDL-cholesterol, so the estimate calculated from triglyceride is used in most settings. This calculation is not valid when the triglyceride is greater than 400 mg/dl (see question 2 above). Increased levels of VLDL-cholesterol have been found to be associated with increased risk of heart disease and stroke.
4. What is non-HDL-cholesterol?
Non-HDL-cholesterol (non-HDL-C) is calculated by subtracting your HDL-C result from your total cholesterol result. It represents the “atherogenic” cholesterol — the cholesterol that can build up in the arteries, form plaques, and cause narrowing of the vessels and blockages. Unlike calculation of VLDL-C (see question 3 above), this calculation is not affected by high levels of triglycerides. Your non-HDL-C result may be used to assess your risk for CVD, especially if you have high triglycerides since high non-HDL-C is associated with increased risk. As recommended by the National Cholesterol Education Program, Adult Treatment Plan III, if you have high triglycerides (greater than 200 mg/dL), the non-HDL-C result can be used as a secondary target of treatments such as lifestyle changes and drugs that aim to lower lipid levels.
Is there anything else I should know?
There is increasing interest in measuring triglycerides in people who have not fasted. The reason is that a non-fasting sample may be more representative of the “usual” circulating level of triglyceride since most of the day blood lipid levels reflect post-meal (post-prandial) levels rather than fasting levels. However, it is not yet certain how to interpret non-fasting levels for evaluating risk, so at present there is no change in the current recommendations for fasting prior to tests for lipid levels.
Article Sources
The Male Hormone Panel
The aging process is inevitable. However, restoring lost male vitality is within reach. The hormones involved in this restoration can now be collectively measured in one salivary panel using the Regular or Expanded Male Hormone Panels (MHP and eMHP). The problems that concern men that most can be grouped into 3 categories:
Vigor:
- loss of sense of well being
- difficulty concentrating
- depression
- irritability and nervousness
- alternation in behavioral patterns
- change in sleep habits/insomnia
Vitality
- decrease in hair density
- reduction in masculinity
- decrease in muscle mass and strength
Virility
decline in sexual function and interest, diminished libido and erictile dysfunction (ED)
- decrease in bone mass (osteoporosis)
Andropause
At around puberty, the important male hormone, testosterone , reaches adult levels. For a long time it was believed that men maintain adequate levels of testosterone throughout life. Many men in their fifties or older however, experience a progressive decline in their energy, vitality, sexual performance and mental capacity. This decline has been labeled "Andropause ." The causes of andropause are believed to be a reduction in testosterone and other androgens. The testicles show a progressive annual drop of 1-1.5% in testoterone output after age 30. Furthermore, as men age, a 1-2% in both Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) has been documented. The clinical manifestations of andropause usually lag ten to twenty years behind the onset of hormone decline. Statistically, andropause effects at least 40% of men ages 55-65, and up to 80% of those aged 65 years or more.
Knowing the levels of the 6-8 hormones measured in the Male Hormone Panels helps you formulate an effective plan to relieve andropausal symptoms.
Regular Male Hormonal Panel (MHP)
Several years ago, Diagnos-Techs, Inc. introduced the first salivary Male Hormonal Panel which evaluates the androgen pathway by measuring the free fractions of the hormones shown below.
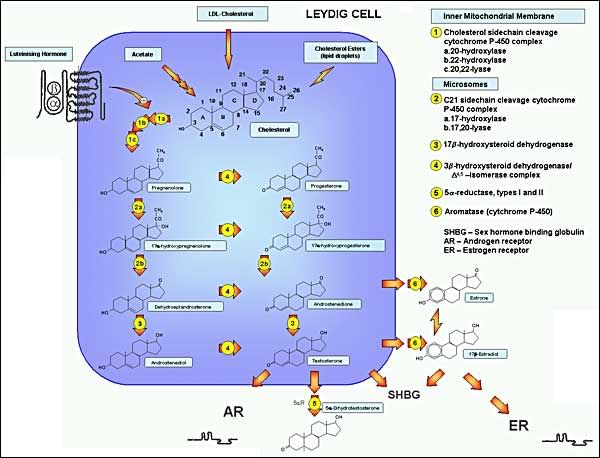
FIGURE 1. Pathways of testosterone biosynthesis and action. In men, testosterone biosynthesis occurs almost exclusively in mature Leydig cells by the enzymatic sequences illustrated. Cholesterol originates predominantly by de novo synthesis pathway from acetyl‚€‘CoA with luteinizing hormone regulating the rate‚€‘limiting step, the conversion of cholesterol to pregnenolone within mitochondria, while remaining enzymatic steps occur in smooth endoplasmic reticulum. The ÔĀ„5 and ÔĀ„4 steroidal pathways are on the left and right, respectively. Testosterone and its androgenic metabolite, dihydrotestosterone, exert biological effects directly through binding to the androgen receptor and indirectly through aromatization of testosterone to estradiol, which allows action via binding to the ER. The androgen and ERs are members of the steroid nuclear receptor superfamily with highly homologous structure differing mostly in the C-terminal ligand binding domain. The LH receptor has the structure of a G-protein linked receptor with its characteristic seven transmembrane spanning helical regions and a large extracellular domain which binds the LH molecule which is a dimeric glycoprotein hormone consisting of an α subunit common to other pituitary glycoprotein hormones and a β subunit specific to LH. Most sex steroids bind to sex hormone binding globulin (SHBG) which binds tightly and carries the majority of testosterone in the bloodstream.
1. Progesterone is a precursor to all androgens and is a physiologic modulator of DHT production
2. DHEA & DHEA-S, the main adrenal androgens are the precursors to both testerone and estradiol, and the limiting factor in their production especially under stress.
3. Androstenedione, another adrenal androgen and precursor to estrone is freely inter-convertible with testosterone.
4. Estrone is the major estrogen in mend and is the product of peripheral aromatization of androstenedione in fat and muscle tissue.
5 & 6 Testosterone, the dominant testicular androgen, is the precursor to 5-dihydrotestosterone (DHT). The androgenic effect in various tissues is not exerted by testosterone buy by the locally produced DHT.
Expanded male hormone Panel (eMHP)
This panel includes all the 6 tests in the regular MHP, plus FSH and LH. Sallivary quantitation of FSH and LH is a technological breakthrough that seperates Diagnos-Techs from the crowd of copycat laboratores. Testosterone and sperm production in males are the equivalent of estrogen and ovulation in females. The pituitary neurohormones, FSH, and LH, stimulate and regulate sperm atogenesis and testosterone production respectively.
- Early detection of an increase in FSH and LH levels is indicative of a progressive decline in male sexuality and functionality. The clinical utility of the Male Hormone Panel is shown in the:
- Measuring of baseline hormones
- Diagnosing andropause and hypogonadism
- Therapeutic monitoring of HRT
- Balancing of hormones
- Investigating of prostate hypertrophy, thinning of hair and hirsutism
- Evaluating of low-libido in both sexes
Beneficial Effects
Following the use of MHP/eMHP, treatment plans using hormones to replace the balance of endogenous production usually produce several positive effects:
- Increase of fitness and sense of well-being
- Decrease of body fat and increase in lean body mass
- Resolution of hormone dependent libido problems
- Prevention of hair thinning
- Increase of hematocrit and RBC counts
- Mitigation of esteoporosis and stimulation of bone formation
- Decrease in total cholesterol, increase in HDL
*Note* Unmonitored male HRT may account for increased incidence of prostatic complications, liver cancer, and accelerated atherosclerosis.
-Diagnos-Techs. INC.
David J Handelsman MB BS, FRACP, PhD Director, ANZAC Research Institute & Department of Andrology, Concord Hospital, Professor of Reproductive Endocrinology & Andrology, University of Sydney,Sydney, NSW 2139, Australia
NOTE: This article is based on research that utilizes the sources cited here as well as the collective experience of the Lab Tests Online Editorial Review Board. This article is periodically reviewed by the Editorial Board and may be updated as a result of the review. Any new sources cited will be added to the list and distinguished from the original sources used.
Sources Used in Current Review
(September 2002) National Heart, Lung, Blood Institute. National Cholesterol Education Program Guidelines, Cholesterol, ATP III. II.3-b, II.9-c. PDF available for download at http://www.nhlbi.nih.gov/guidelines/...l/atp3full.pdf through National Heart, Lung and Blood Institute. Accessed June 2009.
American Heart Association. Guide to primary prevention of cardiovascular diseases: Risk intervention, Blood Lipid Management. Available online at Primary Prevention in the Adult through American Heart Association. Accessed June 2009.
(Updated December 19, 2008) American Heart Association. What your Cholesterol Levels Mean. Available online at What Your Cholesterol Levels Mean through American Heart Association. Accessed May 2009.
American Academy of Family Physicians. Cholesterol: What Your Level Means. (Updated October 2007). Available online at Cholesterol: What Your Level Means -- familydoctor.org through familydoctor.org Home -- familydoctor.org. Accessed September 2008.
(May 12, 2008) Medline Plus Medical Encyclopedia. Coronary Risk Profile. Available online at Coronary risk profile: MedlinePlus Medical Encyclopedia. Accessed October 2008.
ARUP Consult. Physicians Guide. Lipid Panel, Extended. Available online at Lipid Panel, Extended : ARUP Lab Tests through ARUP Laboratories: A National Reference Laboratory. Accessed October 2008.
Clarke, W. and Dufour, D. R., Editors (2006). Contemporary Practice in Clinical Chemistry. AACC Press. Washington, DC. Pp 251-253.
Pagana K, Pagana T. Mosby's Manual of Diagnostic and Laboratory Tests. 3rd Edition, St. Louis: Mosby Elsevier; 2006. Pp 351-356.
Sources Used in Previous Reviews
Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA (2001) 285: 2486-2497.Last edited by HawaiianPride.; 10-20-2010 at 09:51 AM.
-
06-27-2010, 04:34 PM #2
good info
-
06-27-2010, 08:04 PM #3
Thanks. Should be of help to some.
-
06-30-2010, 06:53 AM #4
Wow, great post!!! Cough...sticky... Cough.
-
06-30-2010, 08:59 AM #5
good info,
though i suggest the inclusion of a hormone profile which is also very important which you may have accidently left out.
-
07-03-2010, 07:21 PM #6
yeah with the tes panel explanation this would def be stickey material
-
09-06-2010, 07:46 AM #7
-
09-06-2010, 09:08 AM #8
The Male Hormone Panel
The aging process is inevitable. However, restoring lost male vitality is within reach. The hormones involved in this restoration can now be collectively measured in one salivary panel using the Regular or Expanded Male Hormone Panels (MHP and eMHP). The problems that concern men that most can be grouped into 3 categories:
Vigor:
- loss of sense of well being
- difficulty concentrating
- depression
- irritability and nervousness
- alternation in behavioral patterns
- change in sleep habits/insomnia
Vitality
- decrease in hair density
- reduction in masculinity
- decrease in muscle mass and strength
Virility
decline in sexual function and interest, diminished libido and erictile dysfunction (ED)
- decrease in bone mass (osteoporosis)
Andropause
At around puberty, the important male hormone, testosterone , reaches adult levels. For a long time it was believed that men maintain adequate levels of testosterone throughout life. Many men in their fifties or older however, experience a progressive decline in their energy, vitality, sexual performance and mental capacity. This decline has been labeled "Andropause ." The causes of andropause are believed to be a reduction in testosterone and other androgens. The testicles show a progressive annual drop of 1-1.5% in testoterone output after age 30. Furthermore, as men age, a 1-2% in both Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) has been documented. The clinical manifestations of andropause usually lag ten to twenty years behind the onset of hormone decline. Statistically, andropause effects at least 40% of men ages 55-65, and up to 80% of those aged 65 years or more.
Knowing the levels of the 6-8 hormones measured in the Male Hormone Panels helps you formulate an effective plan to relieve andropausal symptoms.
Regular Male Hormonal Panel (MHP)
Several years ago, Diagnos-Techs, Inc. introduced the first salivary Male Hormonal Panel which evaluates the androgen pathway by measuring the free fractions of the hormones shown below.
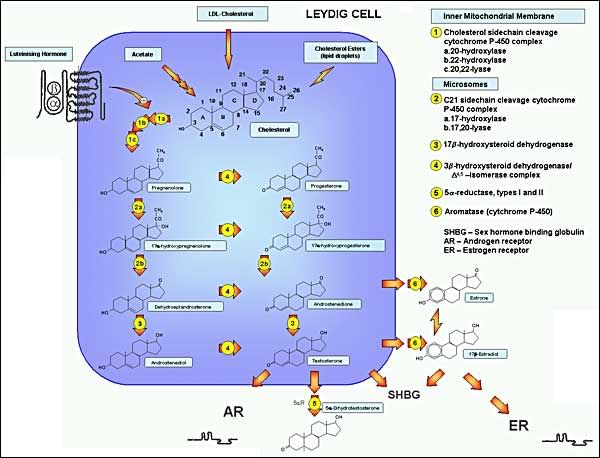
FIGURE 1. Pathways of testosterone biosynthesis and action. In men, testosterone biosynthesis occurs almost exclusively in mature Leydig cells by the enzymatic sequences illustrated. Cholesterol originates predominantly by de novo synthesis pathway from acetyl‚€‘CoA with luteinizing hormone regulating the rate‚€‘limiting step, the conversion of cholesterol to pregnenolone within mitochondria, while remaining enzymatic steps occur in smooth endoplasmic reticulum. The ÔĀ„5 and ÔĀ„4 steroidal pathways are on the left and right, respectively. Testosterone and its androgenic metabolite, dihydrotestosterone, exert biological effects directly through binding to the androgen receptor and indirectly through aromatization of testosterone to estradiol, which allows action via binding to the ER. The androgen and ERs are members of the steroid nuclear receptor superfamily with highly homologous structure differing mostly in the C-terminal ligand binding domain. The LH receptor has the structure of a G-protein linked receptor with its characteristic seven transmembrane spanning helical regions and a large extracellular domain which binds the LH molecule which is a dimeric glycoprotein hormone consisting of an α subunit common to other pituitary glycoprotein hormones and a β subunit specific to LH. Most sex steroids bind to sex hormone binding globulin (SHBG) which binds tightly and carries the majority of testosterone in the bloodstream.
1. Progesterone is a precursor to all androgens and is a physiologic modulator of DHT production
2. DHEA & DHEA-S, the main adrenal androgens are the precursors to both testerone and estradiol, and the limiting factor in their production especially under stress.
3. Androstenedione, another adrenal androgen and precursor to estrone is freely inter-convertible with testosterone.
4. Estrone is the major estrogen in mend and is the product of peripheral aromatization of androstenedione in fat and muscle tissue.
5 & 6 Testosterone, the dominant testicular androgen, is the precursor to 5-dihydrotestosterone (DHT). The androgenic effect in various tissues is not exerted by testosterone buy by the locally produced DHT.
Expanded male hormone Panel (eMHP)
This panel includes all the 6 tests in the regular MHP, plus FSH and LH. Sallivary quantitation of FSH and LH is a technological breakthrough that seperates Diagnos-Techs from the crowd of copycat laboratores. Testosterone and sperm production in males are the equivalent of estrogen and ovulation in females. The pituitary neurohormones, FSH, and LH, stimulate and regulate sperm atogenesis and testosterone production respectively.
- Early detection of an increase in FSH and LH levels is indicative of a progressive decline in male sexuality and functionality. The clinical utility of the Male Hormone Panel is shown in the:
- Measuring of baseline hormones
- Diagnosing andropause and hypogonadism
- Therapeutic monitoring of HRT
- Balancing of hormones
- Investigating of prostate hypertrophy, thinning of hair and hirsutism
- Evaluating of low-libido in both sexes
Beneficial Effects
Following the use of MHP/eMHP, treatment plans using hormones to replace the balance of endogenous production usually produce several positive effects:
- Increase of fitness and sense of well-being
- Decrease of body fat and increase in lean body mass
- Resolution of hormone dependent libido problems
- Prevention of hair thinning
- Increase of hematocrit and RBC counts
- Mitigation of esteoporosis and stimulation of bone formation
- Decrease in total cholesterol, increase in HDL
*Note* Unmonitored male HRT may account for increased incidence of prostatic complications, liver cancer, and accelerated atherosclerosis.
-Diagnos-Techs. INC.
David J Handelsman MB BS, FRACP, PhD Director, ANZAC Research Institute & Department of Andrology, Concord Hospital, Professor of Reproductive Endocrinology & Andrology, University of Sydney,Sydney, NSW 2139, Australia
Thread Information
Users Browsing this Thread
There are currently 1 users browsing this thread. (0 members and 1 guests)



 LinkBack URL
LinkBack URL About LinkBacks
About LinkBacks

 Reply With Quote
Reply With Quote






Gearheaded
12-30-2024, 06:57 AM in ANABOLIC STEROIDS - QUESTIONS & ANSWERS